DIABETES SERVICES
Insulin Pump services
- Our staffs have expertise in day-to-day outpatient/inpatient management in delivering optimal care for patients on an Insulin pump.
- Our dedicated team includes a specialized dietitian, diabetes specialist nurses trained in delivering Insulin pump care.

Type 1 Diabetes
In type 1 diabetes, the pancreas produces little or no insulin. People with type 1 diabetes need to therefore replace the insulin with the help of insulin injections (3 to 4 times daily) or an insulin pump. Type 1 diabetes needs careful daily management and Insulin injections should not be omitted as it could lead to life threatening consequences. Type 1 diabetes is managed with:
- Insulin replacement through lifelong multiple insulin injections (4 to 6 every day) or use of an insulin pump
- Monitoring of blood glucose levels regularly with a glucometer
- Following a healthy diet and eating plan
- Taking regular exercise
The aim of diabetes management is to keep blood glucose levels as close to the target range as possible, between 80 to 100 mg/dL (fasting). However, the ranges will vary depending on the individual and an individual’s circumstances.
Keeping your blood glucose level at the optimum range is a careful balance between what food is eaten, physical activity and medication. Blood glucose levels, which are too high, could result in hyperglycaemia or ketoacidosis. Blood glucose levels, which are too low (< 70 mg/dL), could result in hypoglycaemia. It is important to learn about each reaction and respond appropriately. Ketoacidosis is an emergency and you must call emergency services immediately. Monitor blood glucose levels throughout the day and even at night. Keeping your blood glucose levels on target will help prevent both short-term and long-term complications.
At Ashwin speciality hospital your Diabetes Educator/ Diabetes specialist nurse and dietitian will help you learn how to check your blood glucose level, inject insulin and develop a healthy eating and exercise plan that is right for you. All our staff are trained in CGMS (Continuous glucose monitoring systems), Retinal screening with Tele-ophthalmology opinion and Biosthesiometry for Neuropathy.
Type 2 Diabetes
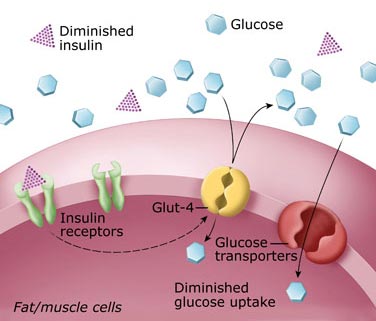
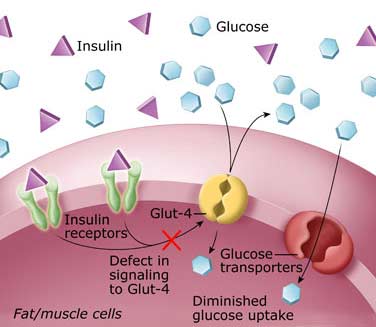
In type 2 diabetes, your pancreas is still working but not as effectively as it needs to. This means your body is building insulin resistance and is unable to effectively convert glucose into energy leaving too much glucose in the blood. Type 2 diabetesis managed through lifestyle modification including a healthy diet, regular exercise, monitoring your blood glucose levels and with regular medications (oral and/or injectable)
Type 2 diabetes is a progressive condition. As time progresses, the insulin becomes more resistant and the pancreas is less effective converting glucose into energy. To help the pancreas convert glucose into energy, people with type 2 diabetes are often prescribed tablets to control their blood glucose levels.
Eventually it may be necessary to start taking insulin to control blood glucose levels. This is when your body is no longer producing enough insulin of its own. Sometimes tablets may be continued in addition to insulin. If you require medication as treatment, it is important to note that this is part of the natural progression of the condition, and taking medication when required can result in fewer complications in the long-term.
The tablets or injections are intended to be used together with healthy eating and regular physical activity, not as a substitute. Occasionally, side effects can occur with medications. Speak with your doctor or pharmacist if you experience any problems. An alternative medication is usually available.
- Eating well helps manage your blood glucose levels and your body weight.
- Exercising helps the insulin work more effectively, lowers your blood pressure and reduces the risk of heart disease.
- Regular blood glucose monitoring tests whether the treatment being followed is adequately controlling blood glucose levels or whether you need to adjust your treatment.
The aim of diabetes management is to keep blood glucose levels as close to the target range between 80 to 110 mg/dL (fasting), and 140 to 160 mg/dL (2 hours post meal). This will help prevent both short-term and long-term complications (heart attacks, stroke, kidney failure, foot ulcers, eye and nerve related problems).
Diabetes in Pregnancy (Gestational Diabetes)

Gestational diabetes is diagnosed during pregnancy when your body cannot cope with the extra demand for insulin production resulting in high blood glucose levels. Regularly monitoring blood glucose levels with a help of a glucometer, adopting a healthy eating plan and performing regular physical activity help appropriate management of gestational diabetes.
Effective management of gestational diabetes will reduce the risk of complications during pregnancy and the birth of your baby. Our healthcare team including your doctor, specialist dietician and diabetes specialist nurses and Diabetes Educators, can help you with blood glucose monitoring, healthy eating and physical activity.
We provide telephone advise on a daily basis, based on the self monitored blood glucose levels (3 to 6 times per day) that is informed to us.
There are three basic components in effectively managing gestational diabetes:
- Monitoring blood glucose levels
- Adopting a healthy eating pattern
- Physical activity
- Regular medications including Insulin
Gestational diabetes can often initially be managed with healthy eating and regular physical activity. However, for some women with gestational diabetes, a few oral medications and insulin injections will be necessary for the rest of the pregnancy. Approximately 10 – 20% of women will need insulin; however, once the baby is born insulin is no longer needed. These insulin injections are completely safe for both you and your baby.
After the baby is born, gestational diabetes usually disappears. A special blood glucose test done before and after intake of a pack of 75g glucose (Oral Glucose Tolerance Test or GTT) is performed six weeks after delivery to ensure that blood glucose levels have returned to normal. However, women who have had gestational diabetes have an increased risk of developing type 2 diabetes later in life and should be tested for diabetes at least every 2 – 3 years.
FAQ ABOUT GESTATIONAL DIABETES
If gestational diabetes is not controlled well and you don’t check your blood glucose levels regularly with a glucometer or ifthe blood glucose levels persistently remain high it may result in problems such as a large baby, miscarriage and stillbirth (baby born without life). A large baby can create the risk of injury at delivery, caesarean delivery, forceps delivery and a need for the baby to be looked after in special care until the glucose level stabilizes after delivery. Other complications may include pregnancy loss and premature delivery. However, if the blood sugars are well monitored and controlled along with a good diet and medications (Insulin) where necessary these risks are extremely low.
It is important to regularly monitor blood glucose levels at home to check that management of gestational diabetes is keeping the blood glucose levels within the target range.
GLUCOSE TARGETS IN PREGNANCY
- Pre meal or Fasting – <93 mg/dL
- 1 hr Post meal – <140 mg/dL
- 2 hr Post meal – <120 mg/dL
The Diabetes Educator or diabetes specialist nurse at Ashwin hospital can show you how to check your blood glucose levels and help you understand your blood glucose patterns. This is to ensure appropriate treatment can be administered and changed as necessary. (eg: change of Insulin doses). The doctor or Diabetes Educator will advise you on recommended blood glucose target levels and testing times during the hospital visit and during telephone reporting thereafter.
If healthy eating and physical activity alone cannot manage your blood glucose levels, your doctor may suggest medication. Most diabetes tablets are not suitable for use during pregnancy, but insulin injections and/or a medication called metformin may be required to help manage your gestational diabetes.
Eating well with gestational diabetes. An important part of managing gestational diabetes relates to diet. Following a healthy eating plan will assist in:
- Managing blood glucose levels within the target range advised by your doctor
- Providing adequate nutrition for you and your growing baby
- Achieving appropriate weight changes during your pregnancy.
Women with gestational diabetes are encouraged to:
- Choose foods that are varied and enjoyable that provide the nutrients you especially need during pregnancy. This means foods which include: calcium (e.g. Milk and cheese), iron (e.g. Red meat, chicken and fish), folic acid (e.g. Dark green leafy vegetables lightly cooked, low in fat, particularly saturated fat(e.g. use oils such as canola, olive and polyunsaturated oils and margarines and use lean meats such as skinless chicken and low fat dairy foods)
- High in fibre
- Completely avoid foods and drinks containing large amounts of sugar, jaggery
- Choose Basmati or parboiled or hand poundrices instead of refined varieties – they have a lower glycaemic index and will help you to stay fuller for longer.
Fat
Try to limit the amount of fat you eat, particularly saturated fat. Use healthy fats like canola, olive and polyunsaturated oils and margarines, avocados and unsalted nuts. To limit your saturated fat intake, select lean meats, skinless chicken and low-fat dairy foods and avoid takeaway and processed foods.

Other dietary considerations
Nutritious foods that will not cause excess weight gain or cause your blood glucose levels to go up can be eaten freely. These foods include fruits such as strawberries, passion fruit, lemons and limes and all vegetables (except potato, corn, sweet potato, taro, beans, lentils and chickpeas). Try to include at least 2 cups of vegetables each day.
Keeping active with gestational diabetes
For women with gestational diabetes, moderate intensity physical activity can help to manage blood glucose levels. ‘Moderate’ means a slight but noticeable increase in breathing and heart rate. If there are no specific obstetric or medical conditions, you should be able to safely exercise during pregnancy. However, it is best to discuss this with your obstetrician prior to commencing any exercise regime in pregnancy.
Benefits of keeping active
Physical activity helps to reduce insulin resistance. Regular exercise, like walking, helps to increase fitness and prepares you for the birth of your baby. Physical activity also helps to keep your blood glucose levels under control.
Remember, before starting or continuing any form of physical activity, always check with your obstetrician or midwife.
It’s never too late to start moving, and there are many ways that you can keep active as a part of your everyday routine. Basically, anything that gets you moving is generally good for your diabetes and will also improve your overall feeling of wellbeing. For example, walking is a great way to move.
Carbohydrates
Carbohydrate foods are broken down into glucose and used for energy. To help manage your blood glucose levels, it is important to spread and limit your carbohydrate foods over the three main meals. Foods that contain carbohydrate include:
- Idli, Dosa
- Multigrain breads and breakfast cereals
- Pasta, rice (preferably Basmati or Doongara) and noodles
- Potato (in moderation) and corn
- Legumes such as baked beans, red kidney beans and lentils
- Fruits (Avoid fruit juices and high glycaemic fruits like banana, mango, dates etc)
- Milks and yoghurts
Carbohydrate foods that contain little nutritional value include sucrose (table sugar), soft drinks, cordials, fruit juices, lollies, cakes and biscuits. These food items need to be completely avoided.
Protein
Include two small serves of protein each day as protein is important for the growth of the baby and maintenance of healthy mum. Protein foods include lean meat, skinless chicken, fish, eggs and reduced fat cheese. These foods do not directly affect your blood glucose levels. Milk, yoghurts, custards and legumes (beans, lentils, and chickpeas) are also important sources of protein. However, remember that they also contain carbohydrate.
Calcium & iron
Calcium and iron requirements increase during pregnancy. Try to include 2-3 serves of low fat calcium rich foods each day (1 serve = 250 ml milk, 200 g of yoghurt or 2 slices of cheese). The iron from red meat, chicken and fish is readily absorbed. However, if you are a vegetarian or do not eat these foods regularly, an iron supplement or pregnancy multivitamin may be required. Discuss this with your doctor or dietician.
Drinks
The best drink for your body is water – try it with fresh lemon or lime for something different. ‘Diet’ or sugar-free drinks are suitable for people with diabetes. However carbonated and caffeinated varieties can increase the risk of osteoporosis and may affect mood so should be consumed in moderation by everyone.
Alternative sweeteners – The use of intense sweeteners by people with diabetes is preferable to use of natural sugars.

After pregnancy
After the baby is born, gestational diabetes usually disappears. A special blood glucose test (Oral Glucose Tolerance Test) (OGTT) is performed six weeks after delivery to ensure that blood glucose levels have returned to normal. However, women who have had gestational diabetes have an increased risk of developing type 2 diabetes later in life and should be tested for diabetes at least every 2 – 3 years.
It is recommended that you check for diabetes after the birth of your baby:
- At least every 2 to 3 years
- Before planning a further pregnancy
- If you’re feeling unwell
Remember that the future risk of developing type 2 diabetes in a lady who had gestational diabetes is as high as 50% in ten years. While maternal blood glucose levels usually return to normal after birth, there is an increased risk for the mother developing type 2 diabetes in the future. To reduce your risk or delay the development of type 2 diabetes, keep in mind the following important points:
- Maintain or achieve a healthy weight. Balancing food intake with activity levels is the best way to maintain or reduce any excess body weight.
- Eat healthily. Limit saturated fat. Choose lean meat, skinless chicken and low fat dairy foods. Limit processed and fried foods. Eat plenty of vegetables, legumes, fruits, wholegrain breads and cereals.
- Be physically active. Aim to include at least 30 minutes of moderate intensity physical activity on most days. You should discuss your physical activity plans with your doctor prior to starting any exercise regime.
Can I breastfeed if I have gestational diabetes?
Breastfeeding is recommended for all women, including women with gestational diabetes. Breastfeeding provides the best start for your baby and can help you to return to your pre-pregnancy weight.
FAQ ABOUT DIET AND DIABETES
Maintaining an ideal body weight adds productive, healthy and happy years to life. Medical research has shown that being overweight increases the risk of heart disease, strokes and cancer. A 5-10% body weight loss has been proven to reduce the progression of pre diabetes to diabetes in upto 6 out of 10 individuals with risk of future diabetes. Studies have revealed that when this is added on to regular physical activity and a healthy diet, it could postpone development of diabetes by even more than 15 years.
Maintenance of weight improves insulin sensitivity and improves blood sugar control, reduces blood cholesterol and protects the heart. An ideal weight in diabetes includes reduction of the waistline and improving the lifeline. An ideal weight prevents progression to complications of diabetes especially heart related complications, strokes, reduced blood pressure and lowered risk of cancers.
The cornerstone of diabetes management revolves around an appropriate diet or medical nutrition therapy. It must be stressed that dietary modifications play a vital role at all stages of diabetes and is compulsory irrespective of oral medications or Insulin being used for treatment. Diet is also an important intervention to prevent diabetes. The greatest long term health benefits occur when modifications are initiated straightaway from the time of diagnosis of diabetes.
Dietary recommendations in diabetes have to be individualised. However, certain basic principles have to be remembered. The total caloric requirement in an Indian setup would include 60% carbohydrates and the remaining equally split between proteins and fats. The importance of dietary modifications ensures a reduced glucose excursion especially in the post meal state which lead to reduced diabetes complications, reduced lipid elevations and ensure weight stability.
Foods with a low glycaemic index and glycaemic load are preferred in individuals with diabetes. Glycaemic index (GI) refers to the measure of the relative impact of carbohydrate containing food on blood glucose elevations (Low GI <55; Medium GI 56-69; High GI >70). Glycaemic load incorporates the quality and quantity of carbohydrate consumed (product of GI and carbohydrate content)
Amongst carbohydrates, simple sugars including sugar syrup, fruit juices, sugary drinks, honey, sweets, toffees, jaggery, ice cream, desserts etc are best AVOIDED due to the high GI causing the blood sugar levels to rise precipituously. Limit consumption of starchy carbohydrates like white rice, white pasta, potatoes, refined wheat flour products and refined grains with a high GI. Complex carbohydrates have more fibre and the glucose excursions are more delayed making them an ideal carbohydrate choice. Brown rice, parboiled rice, whole grain bread, oatmeal, barley and millets are prefered carbohydrates.
Fats should be restricted to <20% of calories with avoidance of saturated fats especially deep fried food with oil, butter and ghee. Fatty red meat, processed snacks, deep fried snacks (pakoras, vada, bajji, samosas), dessert creams and high fat cheeses are to be restricted as these pose risk by raising bad cholesterol and thus block the blood flow to the heart, brain and limbs leading to heart attack, stroke and limb amputations. Milk has a low GI but a low fat milk is ideally preferred. Vegetables contain a lot of fiber and have a low GI with a low glycaemic load and are recommended for people with diabetes. Limitation of the portion size and eating in moderation form an essential part of a diabetes diet.
Some studies have interestingly revealed that a higher consumption of certain fresh fruit like berries, apples and grapes is associated with a lower risk of diabetes in comparison with low fruit eating individuals. High consumption of fruit juices in these studies however, increased the risk towards diabetes.
Eating whole fresh organic fruits are important for people with diabetes. Fruits form an essential source of vitamins, minerals, fibre, flavonoids and antioxidants. All fruits have carbohydrates and they too can elevate sugar levels when consumed. However, this is variable and depends on the total carbohydrate content and glycaemic index of the fruit.
The carbohydrate content of a fruit increases by processing (concentrating and refining), drying (resins) and converting them to juices. All these forms of fruit including ripening have a higher GI which would increase the sugar levels. Fruit juices are devoid of fiber, flavanoids and have a high GI.
Fresh fruits with a low carbohydrate content like berries, apples, pears, papaya, guava, pomegranate and oranges have a low glycaemic index. They form the ideal fruit choices and consumption time is ideally in between major meals instead of snacks and includes 2 to 3 fresh servings.
Some fruits like bananas (30 g carbohydrate) and mangoes (50 g carbohydrate) have a high GI which are equivalent to 6 to 9 spoons of sugar. Ideally these high GI fruits are avoided. If these fruits were to be consumed they would have to be counted as part of the total daily carbohydrate in the meal plan for the day and restricted to 10 to 15g (equivalent of 1/3 banana).
Exercise is a vital lifestyle method, which controls blood sugar levels in diabetes. Exercise or physical activity reduces post meal blood glucose levels by causing an enhanced glucose uptake into the muscles by improving insulin sensitivity. This improved insulin action and blood sugar lowering effect could even last for more that 24 hours after the exercise session.
Muscle contractions during physical activity also take up glucose by an insulin independent mechanism. In the immediate short term this results in lowered glucose levels. If exercise is continued regularly this improves blood glucose for the long term and lowers the HbA1C and benefits the heart by reducing complications.
Exercise for diabetes doesn’t include walking, jogging, swimming, cycling, dancing etc. An increase in physical activity including avoiding prolonged sitting especially in front of a TV, walking upstairs instead of using a lift, gardening, dancing are important and must be a natural way of life.
Exercise intensity should be started gradually and increased in a slow and sequential manner setting realistic goals. The recommended baseline exercise for diabetes is moderate physical activity of 150 minutes per week or 30 to 60 minute sessions on most days of the week. Exercise/physical activity should be fun and enjoyable and should not be considered as a punishment for diabetes.
When choosing the types of exercise speak with your health professional for the ideal options especially if there are heart, kidney and eye related complications of diabetes.
If on Insulin, precautions for a hypoglycaemia (low blood glucose
Foot care and footwear is essential for all people with diabetes. It is important to remember to check the feet before and after exercise especially in individuals with peripheral neuropathy – a complication of diabetes affecting nerves. These individuals have lost the sensory perception at the feet and hence they could injure their feet leading to devastating foot ulcers if they are not careful with their footwear.
Diabetes associations like the American Dibates Association allow alcohol in moderation in diabetes. However, alcoholic beverages are best avoided as they can accelerate diabetes related nerve damage, affect blood sugars by making them erratic and also affect blood pressure. Smoking in diabetes has to be STOPPED completely as it poses the greatest risk for serious complications to the heart and the kidney. SMOKING KILLS by causing an enhanced multi-fold risk for a heart attack. Smoking also worsens blood glucose control and worsens diabetes related eye complications. Smoking also damages the nerves to the arms and legs and decreases circulation to the feet leading to foot ulcers and amputations. Smoking cessation has the greatest health benefit to all subjects irrespective of diabetes and is strongly recommended.
